Dietary Protein for Diabetics
If you’re diabetic you’re likely significantly limiting carbohydrates in your diet. If not, find a new dietician. Because carbohydrates are the primary target for managing blood glucose, it’s easy to forget that the other two macronutrients affect insulin and blood sugar too.
Your body primarily uses two sources of energy. Glucose, primarily sourced from foods containing carbohydrates, and ketone bodies, primarily produced from either dietary or stored fat. The glucose and the other digestible carbohydrates are the first-accessed sources of energy.
If you’re limiting carbs, it’s not long after a meal until your body has depleted the glucose in your diet and any glucose it made from the other carbohydrates in your diet. It then begins searching for another source of energy. Next in line after it has expended that glucose is using any stored glycogen in the liver to make some more glucose or to take protein in your diet and convert that protein to some glucose.
The impact of protein on blood sugar
That’s right. With limited carb intake, your body is soon dumping a little bit of glucose into your blood stream that it created from those steaks you just ate. So, as you can see, when you eat protein-rich foods, you will see your blood glucose rise. It won’t do it as quickly as it does with the carbohydrate-rich foods you eat. Instead of peaking in in one to two hours after the meal, that glucose being made from protein will peak at about 5 to 6 hours.
For diabetics attempting to tightly regulate their blood glucose variability, this five-hour spike must be taken into consideration when planning the timing of your fast-acting exogenous insulin, and perhaps, the timing of your meals.
Understanding that protein includes a glucose production potential is important in understanding your overall diet strategy as well.
There are a few high-profile proponents of carnivore diets that propose an all-meat diet, the “extreme” low-carb diet. Or is it? Let’s take a look at that proposition.
The concept that you can swap carb-free meat for vegetables to achieve lower circulating insulin and blood glucose is a misconception.
Many high-fiber vegetables might have less impact on your blood sugar than an equal amount of protein-rich meat.
In a controlled clinical trial conducted in 2015 by Australian researchers, the affect of protein on blood sugar was tested in a group of Type 1 diabetics. At different times, after fasting, the participants were administered various amounts of both carbohydrate and protein boluses (10g and 20g of carbohydrate (CHO) and 12.5g, 25g, 50g, 75g and 100g of protein) and blood glucose was monitored periodically for five hours. This graph shows the results. [ Paterson MA 2016 – Australia ]
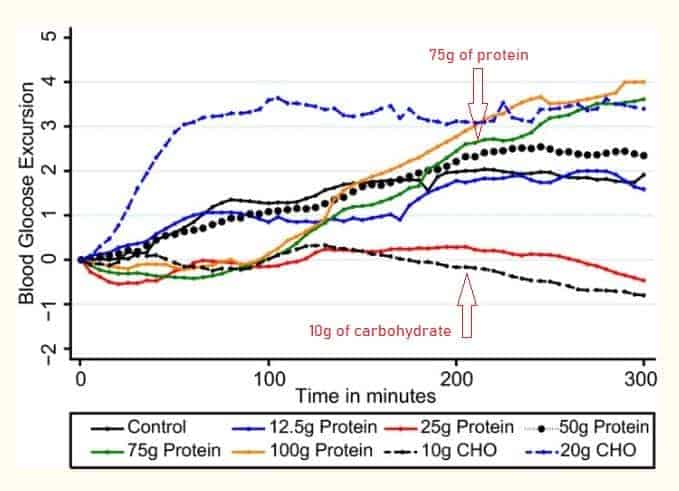
Let’s apply the findings in this study to a real-life example. A 14-oz serving of avocado (about 3 whole fruit) contains a bit more than 7g of digestible carbohydrates (net-carbs). Those three avocados have less than the 10g CHO (carbohydrate) bolus given to the participants in that study. A 14 oz steak, with about 85g of protein, is a bit higher in protein than the 75g of protein given to participants. As you can see, the 10g of carbohydrates (more than what’s in the 14-oz serving of avocado) had zero affect on blood sugar. Yet the 75g of protein caused blood sugar to continuously rise over 5 hours, eventually peaking higher than even a 20g bolus of carbohydrate.
The takeaway
The takeaway is that we have to be cognizant of the fact that protein has a hidden glucose potential since our body will convert it to glucose once dietary carbohydrates are expended. Everyone needs to be cognizant of the potential impact of protein on blood sugar. For Type 1 diabetics, that means taking that delayed blood glucose excursion into account when implementing an exogenous insulin management strategy.

